What is psoriasis?
Psoriasis is a chronic skin disease in which the immune system becomes overactive, causing skin cells to multiply too quickly. As a result, patches of skin become scaly as new skin platelets force older platelets to shed. Psoriasis most commonly manifests on the scalp, elbows, and knees but other parts of the body can also be affected.
Psoriasis can vary significantly in severity and many people with the condition may experience periods with few or no symptoms, followed by periods of “flare-ups”.
There are several types of psoriasis, including:
- Plaque psoriasis: The most common kind of psoriasis, appears as inflamed patches of skin covered by white or grey scales or flakes of skin.
- Guttate psoriasis: Usually affects children or young adults, and appears as small, red dots. It is often linked to upper respiratory infections.
- Pustular psoriasis: This type of psoriasis is less common and mainly affects adults. It causes pus-filled bumps to appear in affected areas.
- Inverse psoriasis: Appears as smooth, red patches in areas with folds of skin, such as armpits, inner elbows, groin, or beneath the breasts.
Erythrodermic psoriasis: A rare, severe form of psoriasis that causes inflamed, scaly skin over most of the body. It often develops in individuals with another form of psoriasis that is not well controlled.
What causes psoriasis?
In people with psoriasis, T-cells, one of the main types of cells used by the immune system, begin to attack healthy skin cells by mistake. This causes the body to produce skin cells more rapidly than usual (producing new skin cells in a cycle approximately every 3 to 7 days, as opposed to every 3 to 4 weeks). This, in turn, triggers the immune system to produce more T-cells.
The exact cause of psoriasis is not fully understood; however, the associated problems with the immune system may be linked to genetics and environmental factors.
Psoriasis and genetics
Psoriasis often runs in families, which means individuals who have a family member with psoriasis may be more likely to develop the condition themselves. Current research indicates a number of genes may be linked to the development of psoriasis; however, having these genes doesn’t always mean you will develop the condition.
Psoriasis and environmental triggers
Psoriasis flare-ups may be linked to external triggers, such as injury to the skin (this is known as the Koebner response), drinking excessive amounts of alcohol, smoking, hormonal changes, stress, certain medications, and suffering from infections or other immune disorders.
What are the treatments for psoriasis?
Topical creams and ointments
Psoriasis treatment can vary depending on the type of psoriasis, the severity of symptoms, and the location of the affected area. However, treatment typically starts with milder therapies, such as topical creams or ointments that are applied directly to the skin. Topical treatments for psoriasis may be purchased over the counter or prescribed by a doctor and can include:
- Emollients
- Steroid creams
- Vitamin D analogues
- Calcineurin inhibitors
- Dithranol
- Coal tar
Phototherapy
In more severe cases, or when the condition isn’t responding well to first-line treatments, patients may be referred to a dermatologist. In these cases, phototherapy, which involves exposing the affected area to different types of ultraviolet light, may be prescribed.
Oral and injected medications
In severe cases or cases in which other treatments have not been successful, systemic treatments may be considered. This can include non-biological (usually in the form of tablets ot capsules) or biological (usually administered as injections) therapies.
Some non-biological systemic medications for psoriasis include methotrexate, ciclosporin, and acitretin. Biological medications can include etanercept, adalimumab, infliximab, and ustekinumab.
While these treatments can be effective, they can also have potentially serious side effects, making constant monitoring essential.
Medical cannabis and psoriasis
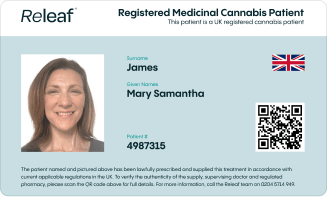
Since medical cannabis was legalised in the UK in 2018, specialist doctors have been permitted to prescribe cannabis-based medicines for a wide range of conditions, including psoriasis. Just like other forms of psoriasis treatment, cannabinoids can be applied topically to the affected area of the skin.
Medical cannabis for psoriasis may now be considered when other treatment options have proven unsuccessful at managing symptoms, or need to be discontinued due to associated side effects. But how could medical cannabis work for psoriasis?
Psoriasis and the endocannabinoid system
The endocannabinoid system (ECS) is a regulatory system, made up of receptors, neurotransmitters, and enzymes, that is expressed throughout our central nervous and immune systems. Cannabinoid receptors within this system can be found in almost all areas of our bodies - including our skin.
Phytocannabinoids, such as CBD and THC, have been found to interact with the ECS to trigger a number of physiological responses, including regulation of pain and inflammation, and oxidative stress.
In recent years, this has led to increased research into the potential of cannabinoids in the treatment of psoriasis. Indeed, past studies have concluded that cannabinoids may be beneficial in reducing inflammation, pain, and itching - all of which are common symptoms of psoriasis.
Moreover, a 2006 study concluded that cannabinoids can inhibit the rapid reproduction of skin cells, “supporting a potential role for cannabinoids in the treatment of psoriasis.” Another study, published in 2019, found that psoriasis patients treated with CBD ointment twice daily experienced significant improvements in their condition.
Commercial CBD products vs medical cannabis for psoriasis
The increased interest in cannabinoids, and CBD in particular, for the treatment of psoriasis, has understandably resulted in many patients turning to commercially available over-the-counter remedies. Indeed, there are many topical CBD products now available in the UK and many other countries. However, it is important to note that these products are not manufactured to the same high standards as approved medical cannabis products.
Final thoughts
Psoriasis is one of the many conditions for which Releaf can prescribe cannabis-based medicines. A growing body of evidence suggests that topical medical cannabis products may be able to provide relief from common psoriasis symptoms where other conventional treatments have failed. Learn more about medical cannabis for psoriasis, and how Releaf works today.